By Dan Ollendorf, PhD, Director, Value Measurement & Global Health Initiatives
The World Health Organization recently released their 2019 list of 10 key threats to global health. Some of these, like the potential for pandemic influenza and the detrimental effects of vulnerable or conflict-ridden settings, make this list seemingly every year. Others are relatively new, such as antimicrobial resistance and vaccine “hesitancy.” One thing is certain – with all of these threats at an urgent or emergent level, countries and health systems need a systematic way to prioritize interventions to address them.
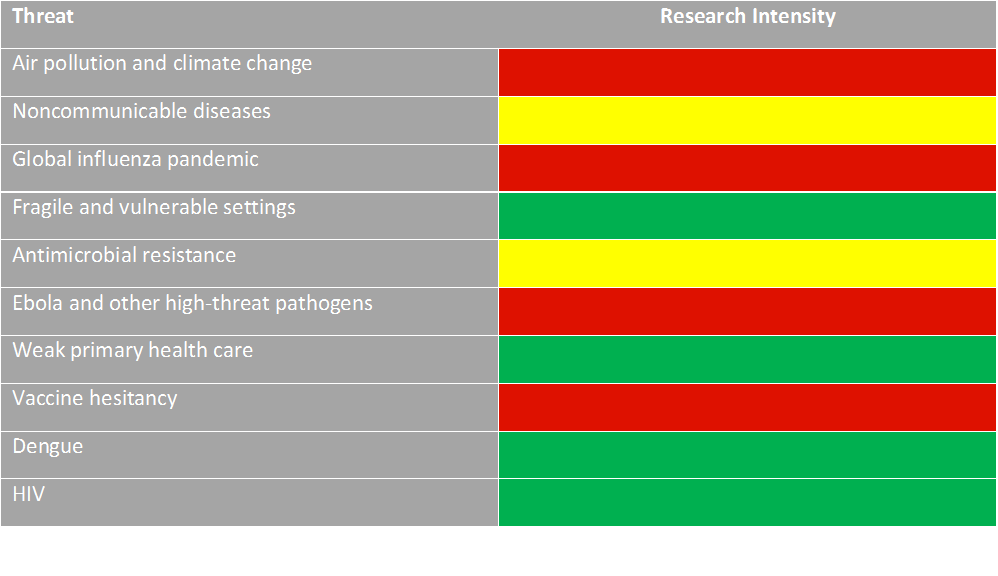
Cost-effectiveness analysis (CEA) is an increasingly accepted tool for prioritization in low- and middle-income settings (LMICs). In some cases, these studies are used to inform the design of a comprehensive essential benefits package at the country level; in others, it is a specific comparison of one type of intervention to another. We examined data from our Tufts Global Health Cost-Effectiveness Analysis (GH CEA) Registry, a standardized, curated database of published studies in LMICs that report results using the cost-per-disability adjusted life year (DALY) averted measure, to understand where research on these threats is more or less abundant. Our resulting “heat table” is presented below.
1. Air pollution & climate change
There has been little published to date on the cost-effectiveness of strategies to address air pollution or the effects of climate change. Most of the environmental interventions contained in our Registry have focused on indoor pollution (e.g., from secondhand smoke) or improvements in general sanitation. With global climate trends changing almost daily, this is an area ripe for economic research, in no small part because raise pollution patterns raise additional equity concerns that should be accounted for.
2. Noncommunicable diseases
According to the WHO, noncommunicable diseases are responsible for 70% of all deaths globally. More importantly, over one-third of these deaths are considered “premature”, and 85% of these premature deaths occur in LMIC settings. While NCD-focused studies are relatively plentiful in our Registry (42% of all interventions), the area remains understudied relative to infectious disease, and several important gaps remain, such as a lack of studies of interventions for diabetes and chronic pulmonary disease.
3. Global influenza pandemic
Despite the ever-present threat of a global influenza outbreak, we identified very few studies examining the cost-effectiveness of immunization against the flu in LMICs, where flu poses particular risks for pregnant women and their unborn children. An example of the benefits of modeling immunization strategies, adjusting for access-to-care concerns, can be found here.
4. Fragile and vulnerable settings
There are enough challenges in prioritizing and allocating health resources in any LMIC; when the sociopolitical context is fragile the challenges become exacerbated. Studies have found, for example, that the countries with the fastest growth in disease burden due to NCDs are the least prepared to deal with this growth. Yet there is reason for hope. Our Registry actually contains many studies focused on fragile settings. A quick look for studies done in Afghanistan, Iraq, Nigeria, Sudan, and South Sudan, four areas of consistently high levels of conflict, identified 71 studies covering a diverse sent of cost-effective interventions, including immunizations, syphilis screenings, drug interventions for malaria, management of childhood pneumonia, dietary fortification of wheat, and others.
5. Antimicrobial resistance
In LMIC settings, the most persistent challenge with antimicrobial resistance is multidrug resistant tuberculosis. We identified 15 studies on this topic from our Registry, covering 71 diagnostic or treatment interventions in multiple settings. There are some clear best practices, as 68 of 71 interventions were found to be cost-saving or highly cost-effective (based on a threshold of 1x GDP per capita in each country).
6. Ebola and other high-threat pathogens
Ebola, Nipah, Zika—the list of emerging threats continues to grow. With their rapid spread, severe and often fatal symptoms, and a lack of effective treatments or vaccines, the most cost-effective intervention may be education, so the general public can be made aware of patterns and vectors of disease spread, warning signs and risk factors, and steps any individual can take in outbreak control. This represents a key opportunity—to both implement an educational intervention before the next outbreak hits and to examine its cost-effectiveness relative to standard practice.
7. Weak primary health care
The Astana Declaration established primary health care as the cornerstone of universal health coverage and access. Already, 119 organizations in 78 countries (and 262 individuals as well) have expressed their commitment to the declaration’s principles. As we’ve previously discussed, the cost-effectiveness of primary and preventive care services has been extensively studied, including screening for major NCD issues such as depression, vision problems, high blood pressure, and cardiovascular disease or stroke.
8. Vaccine hesitancy
Reluctance or outright refusal to undergo vaccination despite its widespread availability is a growing problem in LMICs and high-income countries alike, but there is a significant opportunity to create educational, legal, and policy interventions to reverse this trend in a cost-effective and sustainable fashion. For example, one paper in our Registry concludes that new-generation cholera vaccines are only cost-effective if “herd immunity”) is in effect, something that is only feasible if sufficient numbers of individuals are vaccinated against the disease.
9. Dengue
While Dengue remains a significant scourge throughout LMICs, the effectiveness and cost-effectiveness of routine and/or catch-up dengue vaccination is well-established. In fact, our Registry contains information on nearly 130 dengue interventions, which include vector control programs and multi-disciplinary interventions in addition to various vaccination schedules.
10. HIV
Interventions focused on HIV are among the most well-studied in the GH CEA Registry, comprising approximately 12% of all interventions for all diseases. These include screening, testing, educational and behavioral interventions, and both pharmaceutical and integrated approaches to treatment, and many of them save both money and lives.
It is clear that the top 10 threats for 2019 are described this way for a reason—they are newly emerging or continuously vexing, and managing them is a significant challenge, particularly in resource-constrained settings. But data from our GH CEA Registry suggests deep information on strategies to prioritize in combatting some of these global threats. For other threats, there is a need for new research funding to understand what works, and at what cost.
