By Brittany D'Cruz, BA, Research Associate
Most of the media’s attention is on the impact of mental health disorders in high-income settings, but the reality is that this is a global concern. A significant proportion of the global burden of disease can be attributed to mental health disorders, specifically to neuropsychiatric disorders (e.g., major depression, addiction, ADHD), generating over 160 million person-years of disability worldwide. The gap in access to mental health treatment is particularly pronounced in low- and middle-income countries, where between 76% and 85% of people suffering from severe mental disorders receive no treatment whatsoever. In 2013, the World Health Organization (WHO) released a Mental Health Action Plan to help recognize the essential role of mental health in overall wellbeing and to promote equity through universal health coverage (UHC). Since the release of WHO’s action plan, several countries, including India and Ethiopia, have taken essential steps to provide access to mental health services through UHC. China and Brazil have also embarked on efforts to integrate mental health coverage for citizens with schizophrenia.
When considering inclusion of mental health interventions in UHC, many available interventions may seem unattractive by conventional standards used for prioritizing health interventions. For example, although they contribute significantly to years of life lived with disability, mental health disorders only account for a relatively small share of total deaths globally. In addition, many of the available interventions for mental health are not curative or lifesaving. Because typical mental health services may need to be administered on and off over the course of an individual’s life, they may appear at first glance to place a greater cost and resource burden on the overall healthcare system than other interventions that cure disease.
However, ignoring the potential benefits of providing access to mental health treatment can generate other costs. For example, a 2004 survey in India found that out of pocket expenditures for treatment of psychiatric disorders amounted to almost $280 million. Families who must pay out of pocket for these services may be covering those costs by cutting other types of spending and investments. In addition, it is widely known that mental health disorders, particularly major depressive disorder, can exacerbate the trajectory of other medical conditions and significantly impact productivity in the household and in the workplace. When left untreated, this condition has the potential to lead to increased absences from work and decreased work performance when at work.
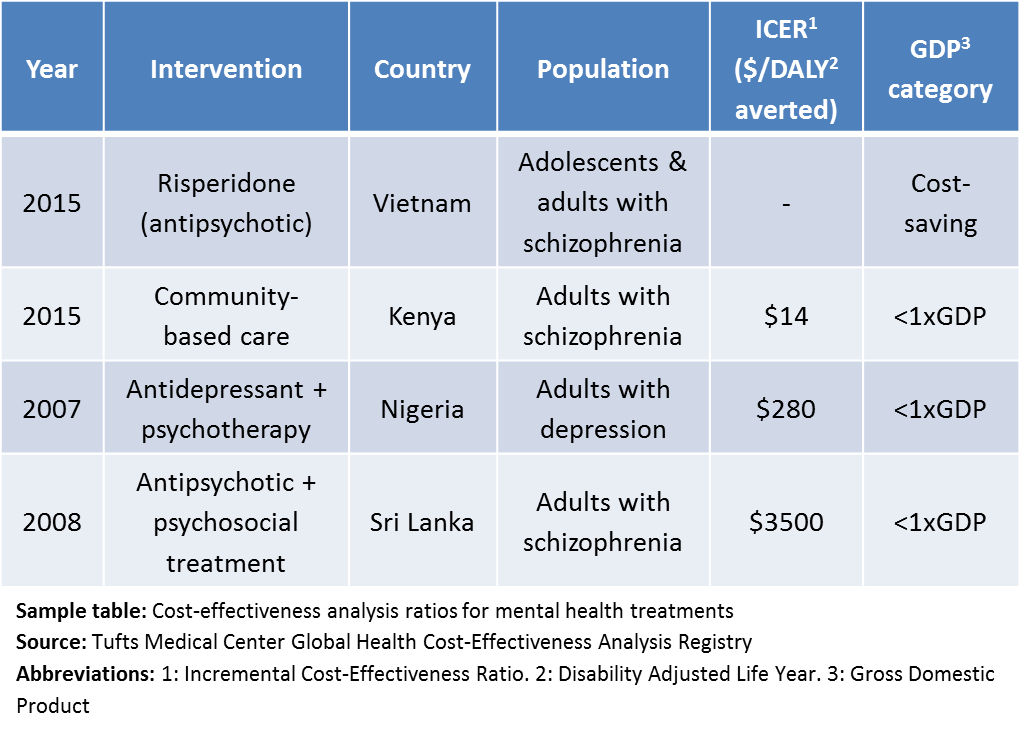
Are there mental health interventions that are worth the investment? Cost-effectiveness analysis is often used in resource-constrained countries to help identify health interventions to include in UHC packages based on how well the added costs of these interventions align with the benefits provided. We were interested in understanding the extent to which the cost-effectiveness of mental health interventions has been assessed in low- and middle-income settings, and whether any high-value interventions have been identified. Based on data captured in the Tufts Global Health Cost-Effectiveness Analysis (GH CEA) Registry, we found over 400 cost-effectiveness results for mental health interventions that were shown to be cost-saving or highly cost-effective (i.e., less than one times the gross domestic product per capita of the target country). Most of these ratios included a combination of some type of pharmaceutical (85%) (e.g., antidepressants) and a health behavior modification (98%) (e.g., psychotherapy or cognitive behavioral therapy) to treat disorders such as schizophrenia, depression, and alcohol use disorders. Some examples are shown in the table below.
 Although there may be additional resource barriers to providing affordable access to mental health services in low and middle income countries, evidence from our Registry suggests that there are some approaches to treat mental health disorders that represent good “value for money” in these settings. Policymakers should take note—whatever their method for prioritization of UHC services, mental health interventions deserve their consideration.
Although there may be additional resource barriers to providing affordable access to mental health services in low and middle income countries, evidence from our Registry suggests that there are some approaches to treat mental health disorders that represent good “value for money” in these settings. Policymakers should take note—whatever their method for prioritization of UHC services, mental health interventions deserve their consideration.
